Share:
Last month, Clinical Corner looked at maintenance and modifications when working with fluid wheelchair cushions. If you missed that article, see Working with Fluid Cushions. This month let's look at the tips and tricks for assessing fluid overfill, underfill, and obliquity fill in fluid cushions.
The easiest way to determine how much of an overfill or underfill is required for an individual is to use an evaluation kit specific to the cushion. An evaluation kit from the cushion manufacturer may contain items like supplemental fluid pads, an insert with a standard fill, and an insert with a 20% underfill. An insert with a standard fill allows a therapist to assess how a client sits on a particular cushion – foam base, fluid insert, and covers(s) – without any modifications to the fluid volume during the equipment assessment. When trialing any fluid cushion, an individual ideally should sit on the cushion for 7 to 10 minutes to ensure bottoming out does not occur.
The therapist determines if there is optimal pelvic immersion into the well of the cushion and optimal pressure distribution through the length of the femurs. If this is the case, fluid modification may not be needed.
To assess for bottoming out, the individual should transfer off the cushion, taking care to not disturb the fluid when transferring from the cushion. The back portion of the cushion cover should be folded over the front of the cushion to expose the fluid pad. Visually observe where the ischial tuberosities and coccyx were positioned on the fluid pad and push down in the depressions with one finger to determine how much fluid is felt before feeling the foam in the well below. There should be at least ½" of fluid before feeling the base of the cushion. 1 If there is not, bottoming out is occurring and an overfill should be considered.
Therapists often question how to determine the correct amount of overfill that is required, balancing the need to ensure bottoming out does not occur while facilitating optimal immersion and pressure distribution. The use of supplemental pads, like the ones shown below, help a therapist to determine how much overfill is required.
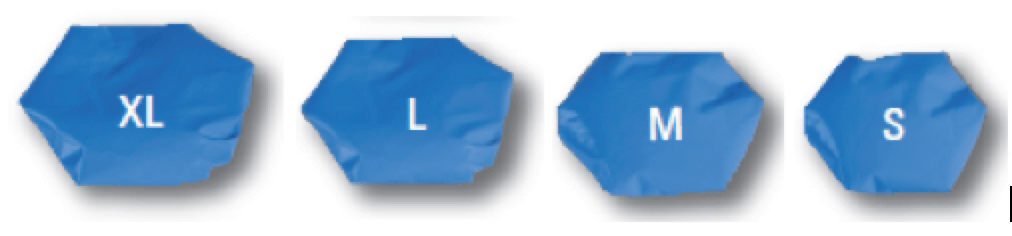
The size of the pad corresponds to a certain amount of fill. For example, 2 extra large supplemental pads are equivalent to 20% overfill; 2 large pads are equivalent to 15% overfill; 2 medium pads are equivalent to 10% overfill; and 2 small pads are equivalent to 5% overfill.
Using a standard insert with a cushion base, the supplemental pads are added to the insert, as shown below.

With the cover on the cushion, the client sits on the cushion with the supplemental pads. At least 7 to 10 minutes should elapse to determine the level of immersion in the cushion. Fluid volume for trial purposes can be adjusted by changing the combination of supplemental fluid pads that are used. A maximum of 40% overfill is available. Once the correct level of overfill is discovered, a modification to fluid volume can be requested on the order form for the final product.
If the client appears to be perched atop of the cushion that has a standard insert, rather than being optimally immersed in the cushion, an underfill likely is needed. The standard fill insert can be replaced with the 20% underfill fluid insert from the evaluation kit for the client to trial during the equipment assessment. 20% underfill is the maximum amount of underfill that can be requested on an order form. If it is determined that a 20% underfill allows for optimal immersion and pressure distribution, a modified cushion can be ordered for the client with a 20% underfill. If it appears that the client needs the fluid volume to be somewhere between a 20% underfill and a standard fluid volume, the supplemental pads from the evaluation kit can be used find the appropriate fluid volume by adding supplemental pads to the underfill insert until optimal immersion is achieved. The various sizes and fluid volumes of the pads allow for 5% increments to the fluid volume. Once the optimal amount of fluid volume is found for an individual, a modified cushion can be ordered for the client, specifying the amount of underfill required.
Positioning for pelvic obliquities can be addressed either through overfills or underfills, depending upon the client's need. If the client needs more fluid to ensure bottoming out does not occur, use an obliquity overfill. Start with the standard insert and add a supplemental fluid pad to the appropriate side, as shown below, and assess the trial with the client.
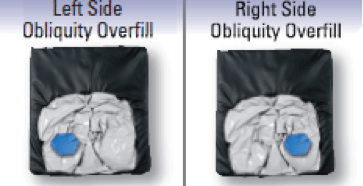
If the client needs less fluid to ensure optimal immersion and the client is not at risk of bottoming out on the cushion, use an obliquity underfill. Start with the 20% underfill insert in the evaluation kit and add supplemental pad(s) to determine the appropriate level of fill on both the right and left sides of the insert.
Another way to address positioning for an obliquity is to use foam obliquity pads. These are ½" closed-cell foam pads that are half-circles and designed to fit in the pelvic well of the contoured cushion, under the fluid insert. The pads are held in place by Velcro and can be stacked to obtain the appropriate height required for the client. If the therapist has obliquity pads in the clinic, these can be trialed with the client to determine the client's response to correction or accommodation of the obliquity.
Summary
The use of an evaluation kit that is specific to a cushion can assist a therapist to determine the amount of overfill or underfill that is required to modify fluid volume based on a client's needs. An obliquity overfill or underfill can be used for positioning, as can closed-cell foam obliquity pads. Simulation of modifications for a client provides confidence when ordering modifications to fluid volume.
Please send your comments, questions, and suggestions for Clinical Corner topics to Sheilagh Sherman, OT Reg. (Ont.) at Sheilagh.Sherman@sunmed.com. Thank you!
References
- JAY® Fusion Cushion Owner's Manual. Retrieved from www.sunrisemedical.ca/seating-positioning/jay/wheelchair-cushions/fusion-cushion#support
Note: The content of this article is not meant to be prescriptive; rather, it is meant as a general resource for clinicians to then use clinical reasoning skills to determine optimal solutions for individual clients. Sheilagh is unable to answer questions from members of the general public. Members of the general public are directed to their own therapists or other health care professionals to ask questions regarding needs.
This article is © Sunrise Medical, Inc., 2022 and cannot be copied, distributed, or otherwise reproduced in whole or in part without the express written permission of Sunrise Medical Canada.